Introduction

Many people have difficulty with nasal congestion and stuffiness. When someone has chronic stuffiness, they’re often forced to breathe through their mouth, leading to a sensation of a dry mouth. In many patients, these symptoms get worse at night when they are lying flat. This can cause them to have less restful sleep.
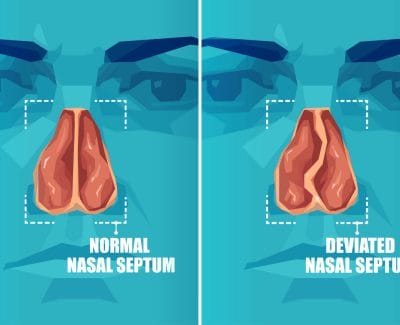
Different types of problems can cause nasal congestion. For example, things like allergies can cause nasal obstruction. Another very common cause of nasal obstruction is narrow nasal passages. Often, narrow nasal passages are the result of problems with the nasal septum and turbinates (See Figure 1).
The nasal septum and the turbinates are normal parts of the nose (See Nasal Anatomy). The nasal septum is the structure that divides the nasal passages into the right and left sides.
The turbinates are also inside the nose, near the septum. There is usually space between the septum and turbinates to allow air to pass through the nose. The turbinates can cause nasal obstruction if they are too large. There are several different types of turbinates in the nose. The ones that most commonly affect airflow are called the inferior turbinates.
Deviated Nasal Septum
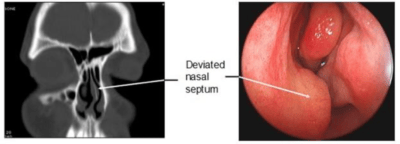
The septum is made of cartilage and bone. The cartilage and bone of the septum are lined by a thin membrane called mucosa. This layer acts like a layer of skin for the inside of the nose. This layer covers and protects the cartilage and bone. It also helps to keep the inside of the nose moist. If the septum is bent or crooked, it is called a deviated nasal septum. When the septum is deviated, one or both sides of the nose can become blocked. In these instances, surgery can help correct the deviation and improve airflow. It’s important to remember that not everyone with a deviated nasal septum needs surgery. However, surgery can be helpful when the deviated septum is causing significant symptoms. The CT scan and picture in Figure 2 demonstrate examples of a deviated nasal septum.
Diagnosis
The diagnosis of a deviated septum can be made by your doctor. Your doctor will perform a thorough evaluation of your symptoms and will examine your nose. You may undergo a procedure in the office called a nasal endoscopy (See Nasal Endoscopy). This will determine the cause of your nasal obstruction. A deviated septum can also be seen on a CT scan. However, a CT scan is often not necessary to diagnose the cause of nasal obstruction. After making the diagnosis, your doctor can discuss treatment options for you. If you have troublesome symptoms, you may be a candidate for surgery to straighten your septum.
Surgery
Surgery to correct a deviated septum is called a septoplasty. Septoplasty is most commonly performed to help relieve nasal obstruction. Sometimes, septoplasty is a necessary part of other surgical procedures.
During a septoplasty, your surgeon will attempt to straighten the cartilage and bone. During the procedure, the lining (the mucosa) is first lifted off the cartilage and bone. The cartilage and bone can then be reshaped. Sometimes, portions of the cartilage and bone need to be removed. The lining is then laid back down.
Even after surgery, the septum is not likely to be “perfectly straight.” The septal cartilage also has a tendency to return to its initial shape and can bend after surgery. But, for most patients, surgery can help straighten the septum so that the nasal passages are more open.
Septoplasty is a procedure that is most commonly done in the operating room under general anesthesia. The procedure is typically performed on an outpatient basis. This means that patients come in and go home the same day. After the surgery you may have splints or packing inside your nose during the healing process. In some instances, there may be nothing more than dissolving stitches inside your nose. Your surgeon can let you know whether splints or packing will be placed in your nose and how long they will stay in place.
Septoplasty involves reconstruction of the cartilage and bone on the inside of the nose. In some situations, patients having septoplasty may also need reconstruction of the outside of the nose. The reconstruction of the outside of the nose is called a rhinoplasty (See Rhinoplasty Overview and Functional). Your doctor can help determine if you would benefit from an external nasal surgery.
Post-Operative Care
You can expect to have fatigue, pain, nasal stuffiness, and mild nasal drainage after your surgery. Pain is generally mild with this type of surgery. It is typically well controlled with over the counter or prescription pain pills. The stuffiness usually results from swelling after the procedure. Stuffiness starts to improve after the first week. You may have drainage of some mucus and blood from your nose after surgery. This is a normal part of the healing process.
You may be asked to use saline sprays or irrigations after your surgery. Please check with your surgeon about any post-surgery care you will need to perform.
Inferior Turbinate Hypertrophy
The turbinates are structures on the side wall of the inside of the nose. They project into the nasal passages as ridges of tissue. They can look like long pillows inside the nose. The turbinates help warm and moisturize air as it flows through the nose. The inferior turbinates can block nasal airflow when they are enlarged (referred to as inferior turbinate hypertrophy). The turbinates are made of bone and soft tissue. Either the bone, the soft tissue or both can become enlarged.
The CT scan and picture in Figure 3 demonstrate examples of inferior turbinate hypertrophy. You can see that enlarged inferior turbinates can cause nasal blockage.

Diagnosis
The diagnosis of enlarged inferior turbinates can be made by your doctor. Your doctor may perform a procedure in the office called a nasal endoscopy (See Nasal Endoscopy). This will determine the cause of your nasal obstruction. After making the diagnosis, your doctor can discuss treatment options for you. If the turbinates are swollen, your doctor may recommend medications for you. For many patients, medications can help reduce the size of the turbinates and improve their nasal obstruction. If you have troublesome symptoms even after using medications, you may be a candidate for surgery.
Surgery
There are many ways to shrink the size of the turbinates. Surgery is typically called turbinate reduction. Surgery can be performed either in the office or in the operating room. In many instances, turbinate surgery and septoplasty are performed at the same time. It is important that the turbinate not be removed completely. Complete turbinate removal can result in a very dry and crusty nose, sometimes a condition referred to as Empty Nose Syndrome. Sometimes, turbinate tissue will re-grow after surgery and the procedure may need to be repeated. This is preferable to the situation of totally removing the turbinate.
You may hear of many different terms being used when it comes to surgery for the turbinates. Examples of these terms are cauterization, coblation, radiofrequency reduction, microdebrider resection and partial resection. These all refer to different methods of reducing the size of the turbinates. Some of these methods shrink the turbinates without removing the turbinate bone or tissue. These methods include cauterization, coblation, and radiofrequency reduction. In each of these methods, a portion of the turbinate is heated up with a special device. Over time, scar tissue forms in the heated portion of turbinate, causing the turbinate to shrink in size. With some of the other procedures, a portion of the turbinate is removed. It is important that enough of the turbinate remain. This will allow the turbinate to warm and humidify the air that is flowing through the nose. A procedure called submucosal resection is a common technique used to treat enlarged turbinates. With this procedure, the lining of the turbinate is left intact, but the inside of the turbinate is removed. As the turbinate heals, it will be much smaller than before surgery. Sometimes, this resection can be performed with a device called a microdebrider. This device allows the surgeon to remove the “stuffing” through a small opening in the turbinate. In some instances, turbinate bone is removed. After the surgery you may have packing in your nose during the healing process.
Post-Operative Care
You can expect to have fatigue, pain, nasal stuffiness, and mild nasal drainage after your surgery. Pain is generally mild with this type of surgery. It is typically well controlled with over the counter or prescription pain pills. The stuffiness usually results from swelling after the procedure. Stuffiness starts to improve after the first week. You may have drainage of some mucus and blood from your nose after surgery. This is a normal part of the healing process.
You may be asked to use saline sprays or irrigations after your surgery. Please check with your surgeon about any post-surgery care you will need to perform.
Risks of Septal and Turbinate Surgery
As with any surgical procedure, septal and turbinate procedures have associated risks. The chance of a complication occurring is very small. It is important that you understand the potential problems. You should ask your surgeon about any concerns you may have.
Bleeding
Most nasal surgery involves some degree of bleeding, which is generally well tolerated. In very rare situations, significant bleeding may require termination of the procedure. Blood transfusion is rarely necessary and is given only in an emergency. You should stop use of blood thinners such as aspirin, ibuprofen, omega 3 and vitamin E at least one week before surgery. If you require prescription blood thinners, please make sure you discuss this with your surgeon. Your surgeon will provide guidelines on when these medications can be stopped and re- started.
Persistent symptoms
A large majority of patients (over 90%) have improvement in their symptoms after surgery. However, many different factors can impact the final outcome. Some patients may have persistent nasal obstruction after surgery. In very rare instances, patients may notice no improvement or worsening of their nasal obstruction.
Infection
Fortunately, infections after septal and turbinate surgery are very rare. A very rare infection called “Toxic Shock Syndrome” can also occur. This is a life-threatening infection and requires immediate treatment. If you note a change in your blood pressure, heart rate, fever and unusual symptoms of skin changes, please notify your surgeon immediately. The risk of toxic shock syndrome is thought to be less than one case in one hundred thousand septoplasty procedures.
Tooth and nose numbness
Temporary numbness or pain in the teeth after surgery is common. The nerves that go to the gums and front teeth of the upper jaw come through the nose. Surgery on the septum can lead to stretching or injury to these nerves. This can lead to some numbness of the teeth of the upper jaw. In most instances, the numbness is temporary. Similarly, the tip of the nose may be numb after septoplasty. Sometimes, sensation can take weeks or even months to return. Rarely, some patients can have persistent numbness of these areas.
Septal perforation
A septal perforation is a hole in the nasal septum. This can develop during or after surgery. Sometimes, a perforation can lead to bleeding, crusting and obstruction. Great care is taken during your procedure to prevent such a complication, but there is still a small risk this may occur. If the perforation does not cause any symptoms, then nothing further need be done. For symptomatic perforations, surgical closure or placement of a synthetic septal button can be performed.
Brain fluid leak
There is a very rare chance of creating a leak of brain (cerebrospinal) fluid. Should the rare complication of a brain fluid leak occur, it may create a potential pathway for infection. If a brain fluid leak were to occur, hospitalization and likely additional surgery would be necessary. This is an extremely rare problem after septoplasty.
Other uncommon risks of surgery include:
- Change of sense of smell or taste
- Change in voice
- Swelling or bruising of the area around the eye
- Very small risk of a subtle change in the external appearance of the nose after a septoplasty
Common Questions
How can I find out what is causing my nose blockage?
A deviated nasal septum and large turbinates are two of the most common causes of nasal obstruction. However, there are other problems that can cause these same symptoms of stuffiness and difficulty breathing through the nose. For example, problems like polyps can cause nasal blockage. The best way to diagnose the problem is to undergo a nasal endoscopy. This is a painless procedure that is performed in a Otorhinolaryngologist’s (ENT) office. A small endoscope is used to visualize the inside of the nasal passages. This allows your doctor to determine why airflow may be reduced or blocked.
What treatments are available for nasal obstruction?
The treatment depends on the cause of the obstruction. For patients who have swollen turbinates, prescription medications like steroid nasal sprays can help. Over-the-counter decongestant pills (like Sudafed®) can also help. However, using decongestants over the long term is generally not recommended. Some patients may continue to have blockage despite the use of medications and other measures. These patients may benefit from surgery.
How do I know if I would benefit from septoplasty or turbinate surgery?
An otorhinolaryngologist will be able to diagnose the causes of your obstruction. ENT surgeons are experienced in nasal problems and will be able to help you decide if surgery would be helpful.
Will my nose be broken during a septoplasty?
When patients undergo septal and turbinate procedures, the surgery is performed on the inside of the nose. Unless you are having a rhinoplasty procedure at the same time, the surgery will not involve the outside of the nose. So, your nose will not be broken, and any external bruising is very unlikely.
Copyright © 2020 by the American Rhinologic Society