Introduction
Epistaxis is bleeding from the nose. Nosebleeds are caused by the bursting of a blood vessel within the nostril, nasal cavity or nasopharynx. Nosebleeds are rarely life threatening and usually stop on their own. Epistaxis is divided into two categories by the site of bleeding. Anterior nosebleeds are in the front of the nose. Posterior nosebleeds are in the back of the nose.
About 60% of the population has epistaxis at some point. 6% of nosebleeds require medical attention. The cause of epistaxis is often unknown. It may be spontaneous or result from trauma, medications, tumors, or surgery. Environmental factors include changes in weather and humidity. This results in an increase in nosebleeds during the dry winter months.
There is no single definitive treatment for the management of nosebleeds. Many factors play a role in which treatments are used. These include bleeding severity, location, blood thinners, and comorbidities.
The nasal cavity has a large blood supply. Blood is supplied via both the internal and external carotid artery systems. The major arteries are the anterior ethmoid, posterior ethmoid and sphenopalatine arteries. 90% of nosebleeds occur in the anterior inferior (front bottom) septum. The septum is the wall that divides your nose. Anterior nosebleeds occur in an area known as Kiesselbach’s plexus. It was named after Wilhelm Kiesselbach, a German otolaryngologist. Kiesselbach’s plexus is on the anterior nasal septum. It is formed by 5 arteries:
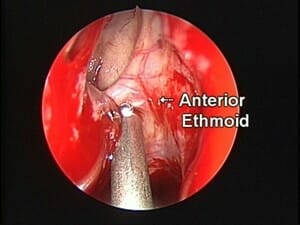
- Anterior ethmoidal artery (a branch of the ophthalmic artery) (See Figure 1)
- Posterior ethmoidal artery (a branch of the ophthalmic artery)
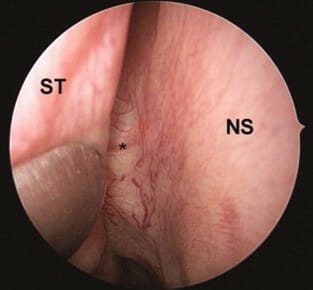
- Sphenopalatine artery (SPA) (a branch of the maxillary artery) (See Figure 2)
- Greater palatine artery (a branch of the maxillary artery)
- Septal branch of the superior labial artery (a branch of the facial artery)
About 5% to 10% of nosebleeds are from the posterior nasal cavity. They arise from an area known as Woodruff’s plexus. Woodruff’s plexus is near the posterior middle turbinate. It consists of branches of the internal maxillary artery. The posterior nasal, sphenopalatine, and ascending pharyngeal arteries also contribute. Posterior nosebleeds usually originate from the lateral wall. They are rarely from the nasal septum. Posterior epistaxis tends to be more brisk and difficult to control.
Etiology
Causes of epistaxis include local, systemic, and unknown causes. Local trauma is the most common cause.
Local Factors
Trauma to the turbinates and septum frequently cause epistaxis.
Nose picking and irritation from nasal sprays cause many anterior nosebleeds. Trauma and fractures of the nose can cause bleeding. Another cause of nosebleeds is infection and mucosal inflammation. Sinusitis, upper airway infections, and allergies can irritate the nose. Septal deviations and perforations can cause irregular nasal airflow. This causes dryness and bleeding in some cases. Sinus, skull base, and orbital surgery can cause severe epistaxis.
Tumors of the nose, sinuses, and nasopharynx can cause recurrent bleeding. Evaluation for this usually includes nasal endoscopy. Imaging studies such as a CT scan may be recommended to screen for tumors.
Recurrent one sided nosebleeds should be evaluated by an Ear, Nose and Throat doctor.
Systemic Factors
Many systemic conditions can cause or contribute to epistaxis.
High blood pressure, telangiectasias (dilated blood vessels), and vasculitis (blood vessel inflammation) are associated with epistaxis.
The use of blood thinners is a frequent contributor. Common blood thinners include aspirin, clopidogrel (Plavix), and warfarin (Coumadin).
Epistaxis can be seen in blood and lymphoproliferative disorders, such as low platelet levels. There can be spontaneous mucous membrane bleeding at platelet levels of 10-20,000. Low platelet levels can result from many things, including cancer. Others causes include chemotherapy, antibiotics, immunodeficiency and an enlarged spleen. Some over the counter medications can cause it as well, like aspirin and NSAIDS. Platelet dysfunction can occur in liver and kidney failure. Vitamin C deficiency can cause platelet problems as well.
Clotting abnormalities can result in recurring epistaxis. Common bleeding disorders include Von Willebrand’s disease, Hemophilia, and Factor XI deficiency. Herbal and alternative medicines can cause clotting abnormalities. For example, Garlic, Ginkgo and Vitamin E may increase the risk of nosebleeds.
Treatment
Direct pressure is usually effective for stopping epistaxis. You should apply pressure to the front, soft part of the nose. Pushing on the high, bony portion will not be effective. Topical nasal decongestants like oxymetazoline can be useful. Applying ointment to the front of the nose daily helps to moisturize the nose. This prevents nosebleeds due to dryness. It is important to avoid any trauma after a nose bleed. Picking scabs or blowing the nose too aggressively can cause another bleed.
Chemical cauterization can be done for control of epistaxis. The chemical used is silver nitrate. It can be done when epistaxis is not controlled by local pressure. This burns the blood vessels shut. When these methods are not effective, packing may be necessary. Packing can be absorbable (dissolves) or non-absorbable (needs to be removed).
For complicated nosebleeds, another treatment is embolization. In this procedure, material is placed within a blood vessel to block it off. This is usually done to the internal maxillary artery. It has a success rate of 71% to 95%, but the procedure has risks. These include stroke, decreased eye movement, and facial nerve weakness. Hematomas (blood clots) can occur at the incision site. Revascularization (reopening of blood vessels) after can occur.
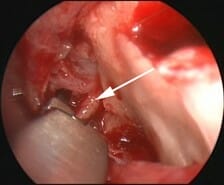
Surgical ligation (tying off the vessel) is an alternative option. The ethmoid arteries can be ligated through an external or endoscopic (through the nose) approach. The SPA is ligated endoscopically. This has been suggested as an ideal treatment for certain nosebleeds. It cuts off the blood supply to the nose at a point closest to the bleeding. This minimizes the risk of persistent bleeding and does not need incisions. Success rates are reported at 92% to 100%. Failures are attributed to not identifying all artery branches. Anticoagulation may contribute to recurrent bleeding as well.
Summary
Non-surgical treatments are effective for most cases of nosebleeds. Pressure, decongestants, packing, and cautery are enough for most nosebleeds. For persistent nosebleeds, embolization and surgery are options. Endoscopic approaches to the SPA and ethmoid arteries have high success rates.
Copyright © 2020 by the American Rhinologic Society

