Introduction
Fungus or fungal allergens is present all around us. It is in the soil, in our homes and in the air we inhale. Indeed, many fungi are part of our normal “microbiome” and help us maintain health. The microbiome consists of bacteria, fungi and other organisms. They are in the gut, on the skin and in the airway. Most healthy people do not react to fungi or fungal allergies if they have a healthy immune system. In rare cases, fungus may cause inflammation in the nose and the sinuses (called fungal rhinosinusitis) just like having mold in sinus cavity symptoms. It may also trigger allergic rhinitis or other allergic diseases like fungal rhinosinusitis which comes in many forms. These forms differ in symptoms, course, severity, pathology and the treatment required. Fungal allergy or fungal sinusitis is broadly classified into invasive and non-invasive types. Invasive fungal sinusitis is extremely rare. Knowing all of this, makes you ask, what kills fungus in the sinuses then?
A simplified classification of fungal sinusitis is as follows:
- Non-invasive fungal sinusitis
- Fungus ball
- Allergic fungal sinusitis
- Non-allergic fungal sinusitis
- Invasive fungal sinusitis
- Acute invasive fungal sinusitis
- Chronic invasive fungal sinusitis
- Granulomatous invasive fungal sinusitis
Non-Invasive Fungal Sinusitis
Fungus Ball
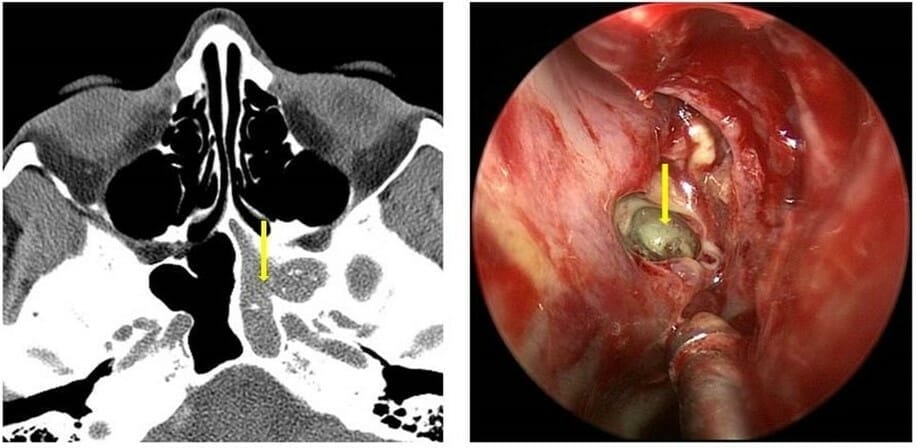
This is a non-invasive form of fungal sinusitis. It is an overgrowth of fungus in the sinuses. Fungal balls most often occur in the maxillary and sphenoid sinuses. Molds such as Aspergillus are typically responsible. The fungus finds favorable conditions for growth, such as warmth and humidity, in the sinuses. Fungal balls elicit very little inflammatory response. Sometimes, the presence of the fungus may lead to bony changes in the wall of the sinus. Occasionally, bacteria can cause infection in the sinus affected by the fungus ball. Patients may have little to no symptom. Fungus balls are often discovered incidentally when a patient has a CT scan for other reasons. The disease has a specific appearance on CT scans and typically, only a single sinus is involved. Treatment is removal of the fungus ball through endoscopic sinus surgery. Usually the fungus has a peanut-butter like appearance (Figure 1). Most patients have excellent results from surgery and may not require further treatment.
Allergic Fungal Sinusitis (AFS)
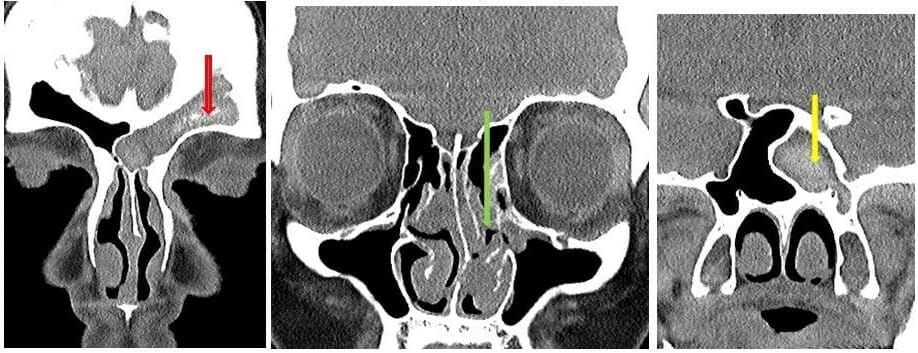
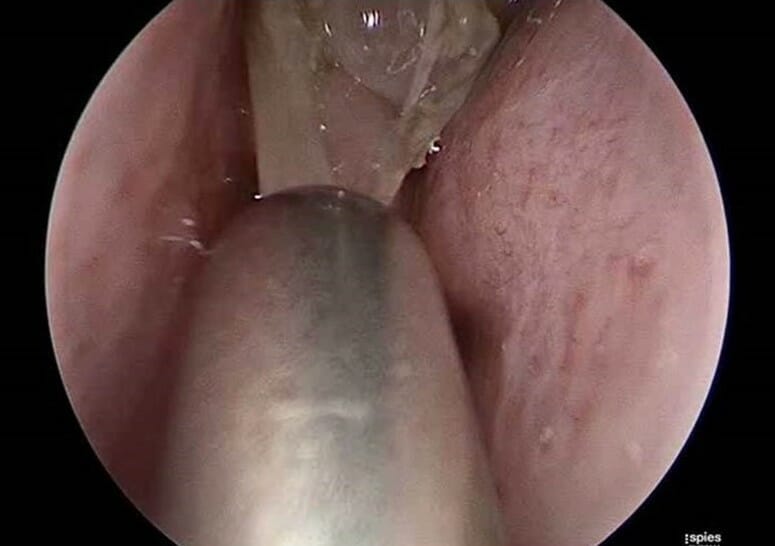
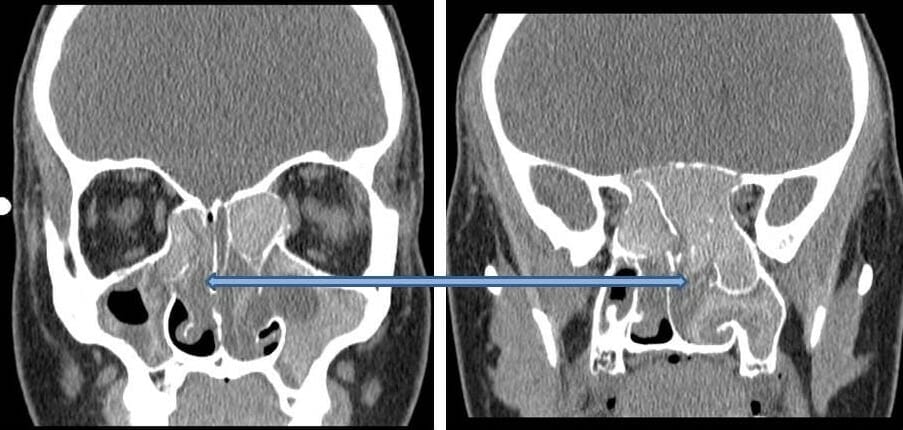
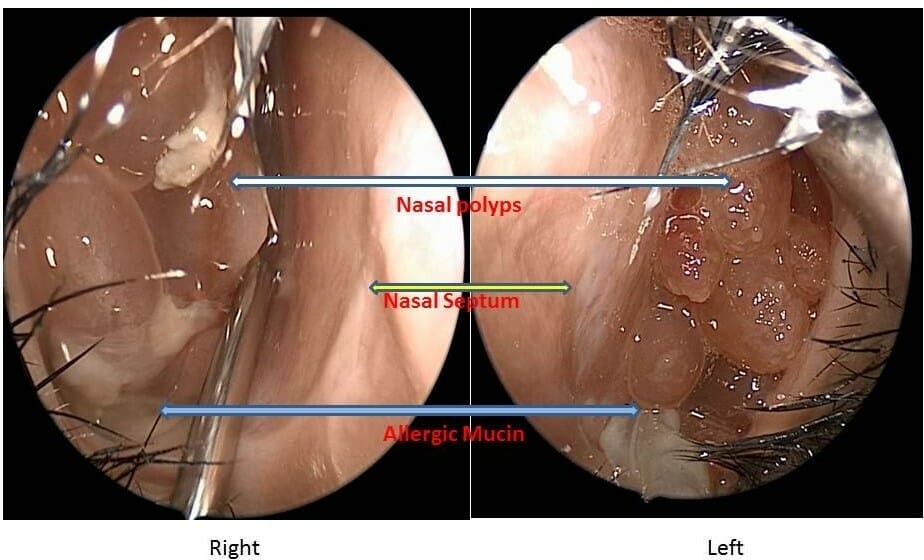
Patients with allergy to certain fungi may develop allergic fungal sinusitis. Common fungi belong to the “Dematiaceous” family. These include Alternaria, Bipolaris and Curvularia species. The presence of fungus in the sinuses causes an allergic and inflammatory response. This results in production of allergic mucin and nasal polyps. Usually, the disease affects more than one sinus on the involved side (Figure 2). However, all sinuses on both sides may be involved in severe cases (Figure 3). Patients have a typical appearance on nasal endoscopy. Allergic mucin and nasal polyps are often visible (Figure 4). Allergy testing to fungi is positive. Sinus CT scans also have a typical appearance (Figure 5). Tissue examination under the microscope shows allergic mucin containing fungal elements. However, the fungus does not invade the tissue. Treatment involves endoscopic sinus surgery. Surgery is necessary to clear the polyps and allergic mucin. It also functions to restore the ventilation and drainage of sinuses. Surgery must be combined with aggressive medical therapy. Corticosteroids are the primary medical treatment. They can be given nasally (spray or irrigation) and/or systemically. Patients may also benefit from treatment of allergy. Immunotherapy (allergy shots or drops) and antihistamines are common forms of allergy treatment. Some patients can have recurrence of nasal polyps and may require further surgery. Long-term follow-up with your Otolaryngologist is therefore recommended. Usually, some form of maintenance medical therapy is needed to control the inflammation long term. Anti-fungal treatment is usually not required because it is the inflammatory reaction to the fungus that needs to be calmed down. However, in severe recurrent disease, anti-fungal therapy may be prescribed.
Non-Allergic Fungal Sinusitis
In some instances, mucin and fungus may be identified in patients without an allergy to fungus. Fungus may also be found in the sinuses of patients that have had previous surgery. Whether these fungi are innocent bystanders or are the cause of sinus disease is currently under investigation.
Invasive Fungal Sinusitis
Acute Invasive Fungal Sinusitis (AIFS)
This is the most dangerous and life-threatening form of fungal sinusitis. Fortunately, it is extremely rare. AIFS usually only affects patients whose immune systems do not function well. These include patients with leukemia, aplastic anemia, uncontrolled diabetes mellitus, and hemochromatosis. Patients undergoing chemotherapy or organ/ bone-marrow transplantation are especially susceptible. Aspergillus or members of the class Zygomycetes (Mucor, Rhizopus) are the most frequent causative fungi. These are opportunistic infections. This means that they typically do not cause harm in healthy people. However, in the susceptible patient, the fungus can grow and rapidly kill sinus tissue and bone over hours or days. This allows the fungus to invade into the surrounding areas of the brain and eye. With nasal endoscopy areas of dead tissue can often be seen. Microscopic examination shows invasion of blood vessels by the fungus. Treatment involves a combination of aggressive surgical and medical therapy. Multiple surgeries may be necessary to remove all dead tissue. Anti-fungal medications are given intravenously. It is also necessary to improve the immune system if possible. All three of these elements are key to improving survival, as this disease is frequently fatal.

Chronic Invasive Fungal Sinusitis
Chronic invasive fungal sinusitis is a slower destructive process. This is unlike AIFS where the typical course is less than 4 weeks. The disease causes rare vascular invasion. There is sparse inflammatory reaction and limited involvement of surrounding structures. It is usually seen in patients with AIDS, diabetes mellitus or those on chronic corticosteroid treatment. The disease most commonly affects the ethmoid and sphenoid sinuses, but may involve any sinus. The typical time course of the disease lasts over 3 months. Tissue cultures show fungus in over half the affected patients. Aspergillus fumigatus is the most commonly grown fungus. Treatment involves surgery in combination with medical therapy. Anti-fungal drugs are given and attempts are made to restore the patient’s immune system.
Granulomatous Invasive Fungal Sinusitis
This form of fungal sinusitis is rare in the United States. It is usually seen in patients from Sudan, India, Pakistan and Saudi Arabia. Patients have normal immune status. The disease has a relatively slow time course. Patients present with an enlarging mass in the cheek, orbit, nose, and/or sinuses. Microscopic examination shows formation of granulomas. This differentiates it from chronic invasive fungal sinusitis. Aspergillus flavus is usually the causative organism. Treatment may involve sinus surgery in combination with anti-fungal drugs.
Summary
In general, fungal infections even nasal yeast infection, rarely affect the nose and sinuses. There are many forms of fungal sinusitis. The most common forms of fungal sinusitis are relatively chronic and indolent. Life threatening fungal sinusitis occurs extremely rarely. Such aggressive disease typically affects severely immunocompromised patients. A complete evaluation by your otolaryngologist will help to determine if you have a form of fungal sinusitis and how it needs to be treated.
Copyright © 2020 by the American Rhinologic Society

