Introduction
Olfaction (the sense of smell) is an important function of the sinonasal cavity. It is increasingly being investigated as it contributes to behavior, cognition, quality of life (QOL), and sinonasal disease. Smelling is critical and important to our daily lives. The sense of smell can alert us to the smoke of a fire or the odor of a natural gas leak. It also detects rotten and spoiled food. Approximately 80% of our taste is related to smell. Remember the smell of your spouse or the taste of your mother’s cooking? Taste and smell unlock some of our deepest memories. They are critical to our perception of the outside world and when lost can negatively affect one’s QOL.
The Relationship Between Taste and Smell
Most patients who complain of a loss of taste actually suffer from a loss of smell. The majority of a food’s flavor comes from our ability to smell it. The tongue is our taste organ, and can sense salty, sweet, sour, bitter, and umami (or savory). The rest of a food’s flavor is provided by our sense of smell. The difference between chocolate and caramel is mostly differentiated by our ability to smell. This is why it is difficult to appreciate a food’s flavor when you have a cold or stuffy nose. Disorders of smell and taste are common, affecting approximately 2 million people in the United States. However, true disorders of only taste are quite rare.
The Anatomy of Smell
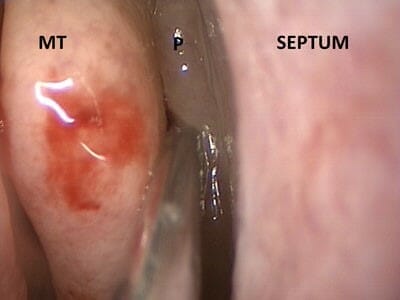
The part of the nose that senses smell is a small area high up in the roof of the nose called the olfactory cleft. Each side of the nose has its own olfactory cleft. Special cells here can sense the various odors carried in the air we breathe. These cells send their signals to the brain via the olfactory nerve.

Causes of Loss of Smell
Loss of smell can result from a physical blockage of the nose or from damage to the olfactory cleft or nerve. Swelling of the nasal lining from the common cold, allergies, sinusitis, and nasal polyps can affect smell. Patients with structural problems like septal deviation and turbinate hypertrophy can have reduced smell. They are more likely to have normal smell compared to those patients who have inflammatory diseases (sinusitis). Patients with nasal polyps tend to have the most severe loss of smell from both inflammation and obstruction. Nasal polyps are small non-cancerous, inflammatory growths in the nose. They block smells from entering the nose. The inflammation from sinusitis can permanently damage the special cells and nerves of the smell pathway. Evidence suggests that by controlling the inflammation in the nose, we can improve the ability to smell.
The loss of smell may be caused by benign or malignant tumors in the nose. Sometimes tumors can grow from the olfactory nerves themselves. Previous radiation treatment to the nose or surrounding areas can cause the loss of smell as a side effect.
Loss of smell can indicate other health problems including obesity, diabetes, high blood pressure and malnutrition. It can be a sign of neurological diseases like Parkinson’s, Alzheimer’s, and multiple sclerosis.
The common cold (See Upper Respiratory Infections) often causes inflammation in the nose. This can impair smell via swelling and obstruction. Usually this loss of smell returns days to weeks after the initial illness has resolved. A few patients experience a more prolonged or permanent loss of smell after a cold. This permanent loss may be caused by inflammation and direct injury of the olfactory nerves by the viruses that cause the cold. Patients without a clear reason for their loss of smell and taste likely have viral-related loss of smell. They may not remember the inciting incident. The virus may have directly attacked the nerves themselves without causing other symptoms of a cold.
There is an association between zinc nasal sprays and sudden and permanent smell loss. These sprays were previously used to try to prevent the flu. Patients who have this type of loss describe an immediate burning sensation when using the spray, followed by loss of smell. The Zicam brand of nasal spray has since been removed from shelves and is no longer available in the United States.
Head trauma can cause injury to the brain or the olfactory nerves causing temporary or permanent loss.
It is also well described that the sense of smell decreases with age, similar to vision and hearing.
There are many other reasons why people may lose their sense of smell. There are metabolic, endocrine, infectious, congenital, developmental and drug-related causes. Your otolaryngologist will know how to look for these other causes.
Testing for Loss of Smell
The physician examining a patient for loss of smell will need to perform an examination of the inside of the nose. This is usually done with nasal endoscopy. The physician will be looking for causes of physical blockage of the olfactory cleft and sources of smell loss.
The physician may use a scratch-and-sniff test to quantify the amount of smell loss a patient has. We call a decreased sense of smell “hyposmia” and complete loss “anosmia”. When there is not an obvious reason for loss of smell, a physician may order a CT or MRI scan. This evaluates the olfactory system from the olfactory cleft to the nerve pathway and brain for abnormalities.
Treatments for Loss of Smell
Treatment for smell loss depends on the cause. If a patient’s loss of smell is caused by allergies or other cause of inflammation, antihistamines or steroids may be recommended. These medications decrease nasal inflammation. Surgery may be suggested if patients have a deviated septum, nasal polyps or other surgically treatable disorders. However, there is no strong evidence to suggest whether surgery or medical management is better for treating smell loss. As mentioned before, certain inflammatory diseases like chronic rhinosinusitis can cause permanent loss. Even with treatment, return of smell to a normal state may not be possible. Many patients who have obstructive causes for their loss of smell report improvements after both medical and surgical treatments. Patients with a loss of smell after trauma or due to a virus unfortunately have limited benefit from available therapies. A short course of oral steroids (ie. Prednisone) may be beneficial in some patients. Recent research has shown that attempting to re-train one’s sense of smell after loss can be beneficial. This is called olfactory training. The nose is exposed to strong, familiar smells several times a day. This may stimulate the unique regenerative capabilities of the olfactory system. It may also rewire the brain’s neural network, similar to physical rehabilitation, to help recover smell. Research is ongoing to determine the exact causes and find additional treatments for smell loss. Other medications that may have some benefit include pentoxifylline, vitamin A, sodium citrate, gabapentin, theophylline, anti-depressants, and long-term antibiotics. Further studies are needed to identify evidence based treatments.
Summary
Patients who suffer from loss of smell or taste are encouraged to seek medical attention. It is best to be seen as soon as possible to determine the cause of the loss. While certain smell losses are permanent, others can be treated medically or surgically. Some of these treatments are more effective if started soon after the onset of loss.
Copyright © 2020 by the American Rhinologic Society

