Introduction
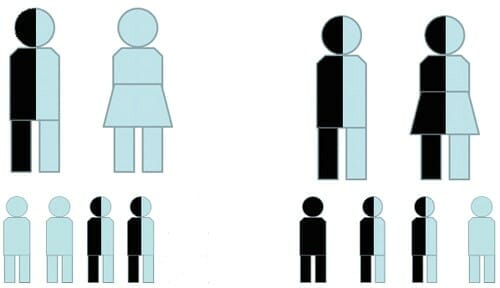
Cystic fibrosis is pronounced “sis-tick fy-broh-sus” and is abbreviated CF. It is a disease that affects multiple systems in the body including the lungs, the digestive tract, and the sinuses. CF is the most common lethal inherited disease in the Caucasian population. It occurs in 1 in 20 newborns. CF is an autosomal recessive inherited disease. Genes or chromosomes come in sets of two. One is inherited from each parent. If a trait or disease is “recessive”, then the expected or “healthy” trait will be expressed if there is at least one normal chromosome. If, however, there are two recessive chromosomes the disease will be expressed. “Carriers” of a recessive trait have one normal and one abnormal chromosome. They do NOT express the diseased trait themselves. Two “carrier” parents have a child who has CF.
Pathophysiology
Secretory glands are found in many organs of the body and produce mucus. Mucus keeps the lining of the organs moist and functions as an immunological barrier. This is seen in the sinuses and lungs. The basic underlying deficit in CF is the lack of a crucial protein (the Cystic Fibrosis Transmembrane Conductance Regulator or CFTR). CFTR allows the transport of ions. It transports chloride and bicarbonate between the cells lining the surface of the respiratory system and the liquid that coats the cells (See Figure). Under normal conditions, the transport of these ions maintains the hydration of the liquid. One of the components of this liquid is mucus. In people who have CF, chloride ions are not well transported across the cell membranes. The mucus then becomes extremely dehydrated and sticky.
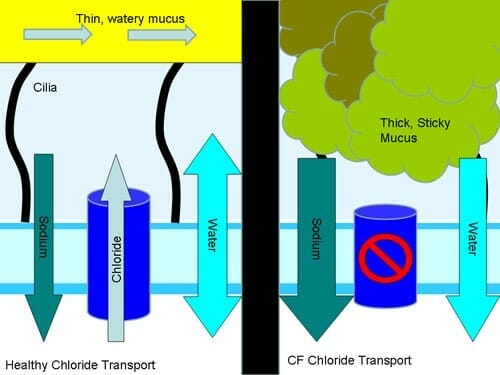
Inside the respiratory system, there are small fingerlike protein projections called cilia. Cilia transport mucus through the nose (See Nasal Physiology) or up and out of the lungs to be swallowed. Pushing very thin and watery mucus is much easier than pushing very thick mucus. In CF the abnormally thick mucus obstructs the smaller airways causing bronchiolitis. This causes permanent scarring in the lungs. The loss of bicarbonate secretion also acidifies the airways. This causes diminished function of the airways natural defenses. Death usually results from respiratory failure.
Nearly all patients with CF will have swelling and thickened mucus in the sinuses that leads to blockage. Infections then develop inside of the sinuses. When swelling becomes severe, polyps may form. Polyps are inflamed watery swellings of the lining of the sinuses that look like grapes. Polyps creates further obstruction in addition to the thick mucus. People with CF may develop significant sinus pain and infections. Also, the bacteria that grow inside of their sinuses can infect their lungs and worsen the lung disease.
In summary, the key steps in the pathophysiology of the disease include:
- A reduction of water in mucus secretions.
- A failure to clear thick sticky mucus secretions.
- Decreased innate immunity of the airway.
- Chronic infections that are particularly localized to the sinuses and lungs.
Symptoms
Symptoms are varied amongst individuals with CF. The earliest sign of CF is meconium ileus. It is seen in approximately 20% of infants with CF. Meconium is the first stool at birth. When it becomes thickened and sticky it can form a mechanical obstruction of the intestine (ileum). This results in abdominal distention and vomiting that needs to be treated urgently. It is common in CF for the pancreas to function poorly (pancreatic insufficiency). This may cause blunted growth and development.
The most common presenting symptoms are respiratory related. They include chronic cough, wheezing, and recurrent upper or lower airway infections. Patients with upper airway manifestations commonly have severe nasal polyposis and thick mucus. Undiagnosed children may have nasal polyposis as their presenting finding. Other symptoms of sinus disease include post nasal drip, constant need to clear one’s throat, headaches, nasal obstruction, loss of taste or smell, and severe bad breath.
Diagnosis
Chest CT or x-ray findings can be very helpful in diagnosing CF. Pulmonary function tests can further evaluate the extent of the pulmonary disease. This test shows low oxygen levels and reduced ability to exhale with increased residual volume in the lungs. The sweat test evaluates for elevated salt (sodium chloride) in the sweat secreted from the skin. Genetic testing is routinely utilized for diagnosis. Genetic testing can also determine suitability for certain drugs, such as the CFTR protein modulator, ivacaftor (see below). Genetic testing should be considered for at-risk family members, but parents often do not know that they are carriers until they have a child with CF.
Management
Currently there is no cure for CF. Patients benefit from a CF team consisting of multiple medical specialists, including pulmonologists and otolaryngologists. Medical therapies like hypertonic saline, intravenous and topical/nebulized antibiotics, and pancreatic enzymes have somewhat alleviated the symptoms of this disease and have helped extend expected life spans of CF patients. Nasal irrigations are particularly helpful in the sinuses to help clear thick sticky mucus. Medical treatment of the sinuses commonly consists of saline irrigations, oral or topical antibiotics, and nasal steroids. Another promising therapy is intranasal nebulized dornase alpha. This medication has shown benefit in several randomized, controlled clinical trials. Surgical treatment of sinus disease could be considered for frequent recurring pulmonary exacerbations, pre or post lung transplant, and/or persistent symptoms such as headaches or nasal obstruction. Endoscopic sinus surgery removes the obstructing nasal polyps and opens the sinuses. This facilitates mucus clearance and allows access for mechanical irrigations. Sinus surgery should be accompanied by postoperative aggressive medical management.
Research efforts dedicated to improving the quality of life and life expectancy of individuals with this debilitating disease are ongoing. Ivacaftor is a CFTR potentiator (channel opener). It was the first CFTR modulator approved by the Food and Drug Administration in January, 2012. This drug has led to significant improvement in the disease manifestations of CF, including pulmonary and sinus disease. Ivacaftor is used for individuals carrying at least one copy of Class 3 CFTR gating mutations (dysfunctional channel opening) and some residual function mutations. Two other CFTR modulators (lumacaftor and tezacaftor) have now been approved for use with ivacaftor. These medications correct F508del CFTR (the most common mutation). Next generation correctors (e.g. VX-445) combined with tezacaftor and ivacaftor (triple combination therapy) have shown very robust improvement over current modulator therapies in current research trials.
Copyright © 2020 by the American Rhinologic Society

