Introduction
Over the past few decades, sinus surgery has evolved significantly. It was once performed through external incisions. It often required extensive nasal packing (i.e. gauze or other material placed in the nose to control bleeding after surgery). Significant pain and a long recovery were common.
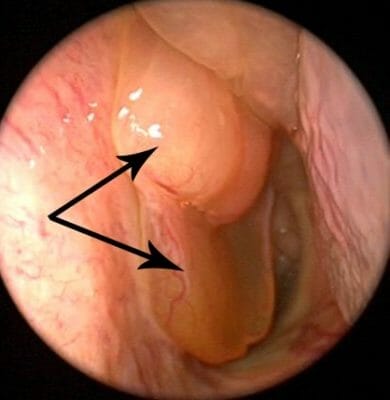
Advances in technology have allowed sinus surgery to be performed entirely through the nose. Incisions on the face or in the mouth are rare. One important development is the nasal endoscope. It is a small, lighted metal telescope placed into the nostril. The endoscope allows the surgeon to see inside the nose and sinuses (See Nasal Endoscopy). Today, endoscopic sinus surgery is typically done with minimal nasal packing, little pain, and short recovery times.

Why Is Endoscopic Sinus Surgery (ESS) Performed?
The most common reason for doing sinus surgery is “chronic rhinosinusitis”/ “chronic sinusitis” (See Adult Sinusitis). Chronic rhinosinusitis is a general term for inflammation (swelling) of the nose and sinuses. (See Nasal Polyps) Chronic means that the inflammation has been present for at least 3 months. The inflammation can be caused by infection, allergies, irritants, and many other things. Many times, we do not know exactly why patients have chronic sinusitis.
Serious infections in the brain or eye might also be a reason for sinus surgery. Nasal polyps are a sign of severe inflammation. They can also be a reason for surgery. ESS is also used to treat select cases of sinonasal tumors, leakage of brain fluid into the nose (See Cerebrospinal Fluid Leak), and eye conditions (See Orbital Decompression and Optic Nerve Decompression). Each individual case is different. Your sinus surgeon will determine if surgery is the best choice for your nasal/sinus problem
What Treatments Should Be Tried Before Endoscopic Sinus Surgery?
Sinus surgery may be recommended when symptoms of sinus inflammation and infection continue even though the proper medical treatments have been tried. Experts generally agree that most patients should be treated with appropriate antibiotics as well as a course of saline irrigations and topical nasal steroids before moving to surgery. It is important to realize that saline irrigations and steroid sprays take time to work, and should be given at least 3-4 weeks of daily use. Patients with polyps may also benefit from a short course of oral steroids, although it is important to discuss the risks and benefits with your physician first. Other medications like topical or oral decongestants can be used every now and then for nasal stuffiness, but should not be used regularly.
Prior to recommending surgery, your physician will likely look into your nose with a small camera (“nasal endoscopy”) to better understand the cause of symptoms, and culture swabs may be used to help choose the most effective antibiotic. If allergies play a role, allergy medications may also be given. Your physician may order a CT scan of your sinuses as part of the work up of a sinus problem that won’t go away.
What Are The Benefits of Endoscopic Sinus Surgery?
When medicines fail to control sinus problems, endoscopic sinus surgery may be helpful. There are several goals of sinus surgery. The main goal is to improve drainage by widening the natural openings of the sinuses. Infected mucus and polyps, if present, are removed. Creating larger sinus openings also allows topical medicines such as steroids to penetrate deeper and control inflammation and swelling.
It is very important to remember that chronic sinusitis is a chronic problem. Surgery has been shown to be very helpful in controlling symptoms and improving quality of life, but in most cases is not a simple “cure”. Surgery is done in addition to, and not instead of, medical treatment of the sinuses. Continuing with medical treatment following surgery is critical to good outcomes. On a practical level, for most patients this means rinsing daily (or more!) with high volume saline and using topical steroids and other medications consistently and as prescribed.
Does Anything Need To Be Done In Preparation For My Endoscopic Sinus Surgery?
Most surgeons recommend that patients avoid any medications that may lead to bleeding, such as NSAIDs (such as ibuprofen), aspirin and blood thinners. In addition, supplements like vitamin E, garlic, ginger, gingko, and ginseng may increase the risk of bleeding. Some patients may be asked to take antibiotics and/or steroids prior to sinus surgery. If you have any questions about which medications you should or should not take, you must ask your surgeon. In most cases, aspirin and other blood thinners should not be stopped before checking with the physician who prescribed the medication.
How Is Endoscopic Sinus Surgery Performed?
Endoscopic sinus surgery (ESS) is typically done in an operating room under general anesthesia, although for some patients certain procedures may be safely performed using local anesthesia (numbing of the nose and sinuses) only. Your surgeon will advise you on the best options for your surgery.
ESS involves the use of small metal telescopes (“endoscope”) to look into the nose and sinus cavities. At the same time, special surgical tools are used to gently remove diseased tissue and enlarge openings into sinuses. These surgical instruments can include typical “cold steel” tools as well as powered devices that cut tissue and suck it away. At times balloons may also be used to widen the sinus openings (See Balloon Sinuplasty). Some surgeons may also perform “image guided surgery”, in which special instruments are connected to your pre-operative CT scan and give live, real-time confirmation of important anatomic landmarks.

Most people have four sinuses on each side of their face, for a total of eight sinuses (See Sinus Anatomy). These are the maxillary, ethmoid, sphenoid, and frontal sinuses. The maxillary sinuses are in your cheek. The ethmoid sinuses are between your eyes. The sphenoid sinuses are almost exactly in the center of your head. Finally, the frontal sinuses are in your forehead. Sinusitis may affect some or all of your sinuses. Your symptoms, examination, and CT scan will determine which sinuses need to be opened. Sometimes during sinus surgery, the nasal septum, which divides the two sides of the nose, is also straightened. The turbinates, which filter and moisten air inside of the nose, may require surgery as well. (See Septoplasty and Turbinate Surgery).
What Is the Recovery After Endoscopic Sinus Surgery?
The use of nasal packing is less common than it was in the past. However, it may still be used in certain cases. Many people do not report much pain after sinus surgery, but every patient is different. Depending on the details of your surgery, you may be prescribed stronger pain medicine, although often over-the-counter acetaminophen (Tylenol) is enough to control minor discomfort. For most patients, pain, congestion, and drainage improves after the first few days. Mild symptoms sometimes linger for several weeks after the surgery. It is again important to remember that control of sinus inflammation requires good, long-term medical management, including after surgery. Your surgeon may place you on medications after surgery and may see you regularly to clean out any crusting or secretions and determine if other treatment are needed. Saline rinses, steroids, and antibiotics are common and should be used just as prescribed.
Your surgeon will provide specific instructions as to what activities are allowed and what must be avoided. In general, excessive pressure to the head should be avoided. Instructions commonly include not blowing the nose, avoiding bending over and lifting heavy weights, keeping the head elevated and adhering to light activity.
Will Endoscopic Sinus Surgery Improve My Symptoms?
Most patients who have endoscopic sinus surgery do very well, with significant improvement in their symptoms and quality of life. Good use of prescribed medications and regular post-operative care is extremely important to having the best possible outcomes.
What Is “Sinuplasty” (A.K.A Balloon Sinuplasty or Balloon Dilation)?
“Sinuplasty” refers to a procedure to dilate the sinus openings with a balloon. Sinuplasty may be a less invasive alternative to ESS in certain situations. It is important to talk with your surgeon to determine the best option to treat your sinus disease.
What Are the Potential Complications of Endoscopic Sinus Surgery?
Complications of sinus surgery are rare and include bleeding, scarring in the nose, failure to improve, and further surgery. Patients with certain types of sinusitis including those with severe polyps, cystic fibrosis, aspirin-exacerbated respiratory disease, and allergic fungal sinusitis, as well as those with severe asthma and a history of prior sinus surgery, are more likely to require a revision procedure. The most serious complications of sinus surgery relate to damage to important structures around the sinuses, including the eye and brain. Although extremely rare, these can include vision loss, brain injury, and CSF leak. If you are uncomfortable with the risks of sinus surgery, it is important that you discuss this with your surgeon.
What Are the Alternatives to Endoscopic Sinus Surgery?
Continued medical therapy is an option, although disease control may be difficult in some cases without surgery. If you are uncertain, it is very reasonable to get a second opinion from another doctor before deciding whether or not to proceed with surgery.
What Is Endoscopic Skull Base Surgery?
Endoscopic skull base surgery is a technique similar to ESS except that the surgery is focused on removing tumors or fixing problems located at the junction of the brain and face, and/or in the brain itself. Like sinus surgery, cameras, video equipment, and other instruments allow the surgeries to be completed entirely through the nose without any facial incisions. For many patients, endoscopic skull base surgery can result in equivalent outcomes to traditional open approaches, with less pain and shorter hospital stays. While this type of surgery is an attractive option, it must be emphasized that this technique is not for all patients or tumors. Care for skull base diseases can be complex, and is often best provided by multi-disciplinary teams of surgeons in high volume centers. Your surgeon will be able to tell you if you are an appropriate candidate.
Copyright © 2020 by the American Rhinologic Society

