Introduction
The normal functions of the nose include respiration, conditioning inspired air, vocal resonance, olfaction, nasal resistance, protection of the lower airway, and ventilation and drainage of the sinuses.
Respiration
The nose is one of natural pathways for breathing (respiration). For basic respiration, humans most often breath through the nose. During inhalation (breathing in), the nose acts as an air conditioning unit. It humidifies, warms, and filters the air in order to facilitate gas exchange in the lungs. Water evaporates from the lining of the nose (mucosa) into the air, bringing the humidity up to 85%. The mucosa also warms the air to body temperature (37 degrees Celsius).
The nasal cycle is the process by which inspired air is warmed and humidified. It is a rhythmic swelling of blood vessels in the turbinates (the ridges that line the nasal cavity). The swelling alternates between the left and right nasal cavities, every 4 hours on average. Sympathetic nerve fibers control the blood flow. Parasympathetic nerve fibers control nasal secretions and mucus production, which is also cyclical. As a result, mucous production is increased on the side with the greater airflow. This process humidifies inspired air. The nasal cycle is normal and is usually not noticed by patients. Patients that do experience alternating nasal obstruction may require evaluation.
Vocal Resonance
The nose also plays a role in speech. The sinuses, which are hollow, air filled spaces, act as a resonance chamber. During phonation of M, N, and NG, the palate remains open. This allows air and sound to pass upwards through the nasopharynx and through the nose. Conditions causing obstruction of the nose or sinuses may affect speech quality, making it hyponasal.
Olfaction
The ability to smell comes from specialized olfactory neuroepithelium. These specialized nerve cells can be found high in the nasal cavity (olfactory cleft). The olfactory cleft is located along the superior portion of the nasal septum and turbinates. As air enters the nasal cavity, a small proportion reaches the olfactory cleft. There, odorant molecules (odors) bind to the nerve receptors. This process sends signals to the brain that result in the sense of smell. Smell is also responsible for our sense of taste. The combination of smell with the five primary tastes (sweet, salty, bitter, sour, umami) results in complex flavors. Therefore, an impaired sense of smell can result in a loss of sense of taste. Problems that affect airflow to the olfactory nerve cells or damage those cells can decrease the sense of smell. Olfactory dysfunction (decreased sense of smell) becomes more common as people age. Olfactory dysfunction affects 50% of people greater than 65 years of age. It is also commonly observed in patients with sinus and nasal diseases. including chronic sinusitis (See Sinusitis Q&A and Adult Sinusitis). Olfactory dysfunction in sinusitis is likely due to both a physical blockage of nasal airflow and damage to the olfactory nerves caused by inflammation.
Filtration of the Airway
The nose is constantly exposed to inhaled debris and microbes (viruses, bacteria, and fungus). The respiratory system has developed several lines of defense to combat this assault. Large particles are trapped by the nasal vibrissae (nose hairs) found at the entrance to the nose (nostrils). Small particles are trapped in the nasal mucus, one of the initial defenses of the airway. Mucus is designed to trap inhaled particles, including microbes. The mucus and trapped debris is then moved down the nose into the throat where it is swallowed. In the stomach the microbes are destroyed by the acidic environment. Mucus is also sometimes removed by sneezing or coughing. These barriers help prevent particles from traveling to the lungs.
Cilia
Mucus is propelled to the throat by the rhythmic beating of very small hair-like structures, known as cilia. Cilia line the airways (Figure 1).
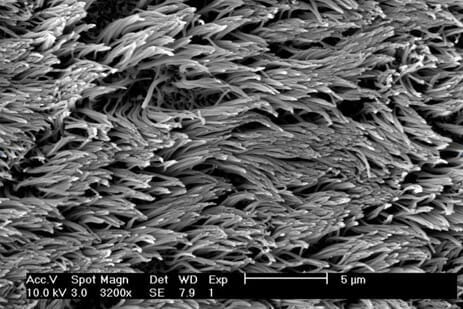
The cilia throughout the nose and sinuses are programmed to beat together in a specific direction. Each sinus has an ostium, which is like a door from the sinus into the nasal cavity. The cilia carry the mucus made by the sinuses towards and through the ostium (See Sinus Anatomy). This natural drainage passage leads to the main hallway that is the nasal cavity. Here, the cilia beat together to drive mucous towards the back of the nose. It then enters the throat through the nasopharynx, where it is eventually swallowed. This process is called mucociliary clearance.
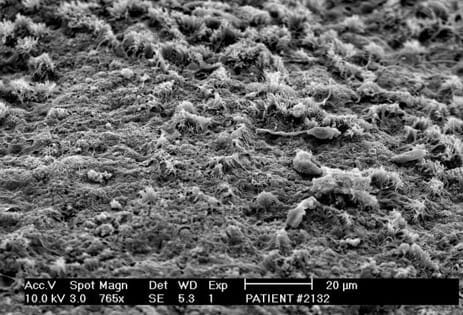
Ciliated cells have sensors that allow them to respond to changes in their environment. For example, if the thickness of the mucous increases, the cilia will increase the speed at which they beat. This allows the cilia to continue clearing the heavy mucous. The same happens in response to an irritating stimulus, to clear the mucous quicker. When the beating of these cilia is impaired, mucociliary clearance does not occur normally. Impaired mucociliary clearance is a known cause of sinus disease. This problem is seen in patients with cystic fibrosis (See Cystic Fibrosis). Impaired mucociliary clearance is also seen in some microbial infections. Toxins produced by some microbes paralyze the cilia. This stops the movement of mucus and optimizes the conditions for infection. Inflammation is the bodies response as it attempts to combat the microbes. Unfortunately, this inflammation can also lead to damage or loss of the cilia (Figure 2). All of which may predispose a patient to future infections and chronic rhinosinusitis. Fortunately, if the microbes are removed and the inflammation is controlled, the cilia can regenerate and resume proper movement of mucus.
While most patients recover from an upper respiratory infection, some go on to develop chronic rhinosinusitis. This is suspected to be due to a combination of factors. A patient’s anatomy, inflammatory response and microbial exposure likely contribute.
Summary
Knowledge of physiology is important to help us understand the diseases that can develop in the nose and sinuses. Descriptions of many of these conditions are available on this website. See Nasal Disorders and Sinusitis and Related disorders.
Copyright © 2020 by the American Rhinologic Society
